ADHD, anxiety, and university students
Struggling with ADHD and anxiety at uni or college? While you may want to do your best, staying on top of assignments, managing unstructured time, and juggling academic and social demands can really affect your ability to focus and concentrate. Learn more about how ADHD affects your uni studies and find tips to help you cope.
Caught in the Perfectionism-Procrastination loop?
Is perfectionism driving you to procrastinate? It may seem counterintuitive, but a fear of failure can stand in the way of you achieving your goals. Read on to learn more…
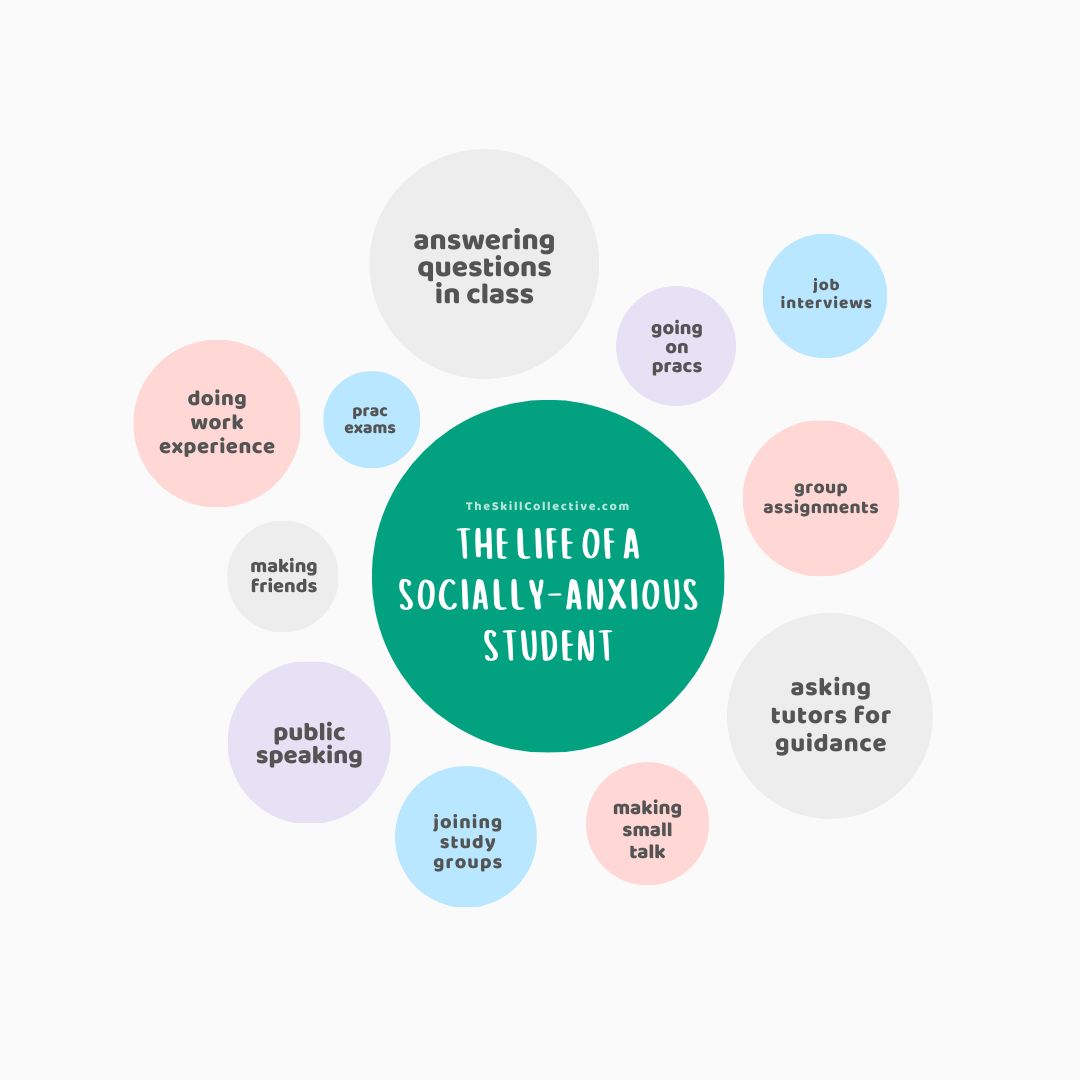
The Life of a Socially-Anxious Student
Living with social anxiety as a student can be challenging - speaking up in class, group assignments, public speaking, gaining work experience, making friends … the list of social situations is endless. But there’s no need to suffer further…read on to find how to go from surviving to thriving in your studies.
How a planner can help you to better manage anxiety
Keep track of your anxiety by monitoring your mood and sticking with healthy habits. Here we outline how the humble planner can help you to achieve your goals when it comes to anxiety.
Parental burnout: What is it, how it differs from burnout, and how to bounce back
As rewarding a role that parenting may be, parental burnout is very real - exhaustion, feeling detached from your children, being less effective as a parent, and feeling fed up with the parenting role. Learn what to do to bounce back and improve your relationship with your children.
Working in FIFO: The challenges for mental health (and tips to help)
A FIFO lifestyle presents unique challenges to your sleep, relationships, and mental health. We cover these challenges and suggest tips to help you cope.
Emetophobia - when a fear of vomiting holds you back in life
Emetophobia, or a fear of vomiting, can have a significant impact on everyday life. Here’s a guide to signs of a phobia of vomiting and to treatments that work.